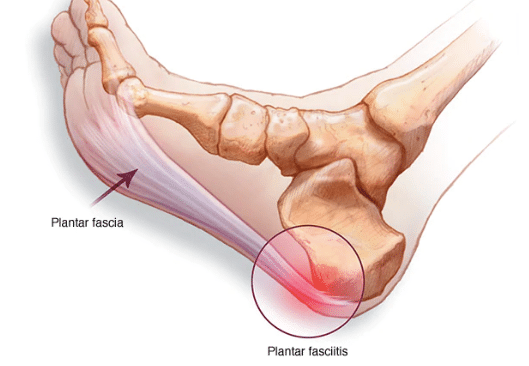
What is plantar fasciitis?
The plantar fascia is the connective tissue that runs along the bottom of the foot from the heel to the toe bones. This makes up the arch of your foot. Plantar fasciitis is the overload of this tissue, and causes pain primarily at the base of your heel, however can occasionally be felt along the line of the plantar fascia.The plantar fascia is an extension of the fascia that connects your calf muscle to your foot. So often an overload or tightness in your calves will contribute to plantar fasciitis.
Common signs and symptoms
Pain in the plantar fascia is typically felt underneath the heel, especially during activities that put stress on the calves, such as walking or running. The discomfort often worsens after periods of rest, feeling more intense in the morning but improving with movement. In some cases, there may be tenderness when touching the base of the heel, and while the pain can vary from day to day, it usually diminishes as you move and the muscles warm up.
How does it happen?
Overload of the plantar fascia can occur in a number of ways, but when daily loads exceed the capacity of the plantar fascia, it will respond in pain.
Overload can occur suddenly, for example a person may jump off a step and feel immediate pain at the base of the heel. Or it can happen gradually over time, such as increasing running kilometers to prepare for a marathon. The accumulative load of progressively running longer distances can eventually exceed the foot’s ability to cope, leading to pain.
Overload can also occur indirectly. For example, if you’re limping because of an injury, you may put extra strain on your uninjured leg. This increased reliance can lead to overuse and ultimately result in pain in the plantar fascia.
Switching footwear can lead to increased strain on the calves, which may, in turn, overload the heel. This is often seen with high heels, where the foot is positioned in plantar flexion, causing the calves to work harder and putting extra stress on the fascia. Additionally, changing to sneakers that promote a more forefoot-striking pattern can also raise the load on both the calves and the plantar fascia.
Hormonal fluctuations can weaken tendons and raise their risk of overuse injuries. For instance, a decrease in estrogen around menopause leads to tendon stiffness, reducing their flexibility and making them more susceptible to injury. As a result, there is an increase in tendinopathies, including plantar fasciitis, among women aged 40 to 60 during the perimenopausal phase.
Additionally, some medications can have a similar effect on tendons, causing degeneration over time without inflammation. This includes statins, which are often prescribed for cholesterol management, and long-term use of steroids to treat inflammation.

How to fix it
1. Pain management
Our initial goal in treating plantar fasciitis is to reduce the pain. There are a number of strategies Physio’s use to aid in pain management.
Firstly we recommend modifying the activities that cause pain. These will often be weight bearing activities such as walking or running, and although it may not be realistic or helpful to completely eliminate these activities from someone’s day, it may be as simple as opting for a lift to work instead of walking to and from the station, or reducing daily walks by half and taking a break from running temporarily.
Plantar fasciitis is typically worse after periods or rest and particularly with your feet resting in a plantar flexed (pointed) position. So a footrest at your desk chair, little exercises to perform at your desk or regularly getting up to move may help in controlling pain.
There are certain taping strategies we can use to better support the plantar fascia which may reduce loading and help with pain. The same goes for arch support in your shoes, or opting for more supportive shoes during the day.
Occasionally other interventions are used to more aggressively manage pain. These can include corticosteriod injections which allow a period of reduced pain, and when used in conjunction with activity modification, strength and mobility, can be a helpful contribution to the overall rehab journey.
2. Mobility
Mobility is an important factor in controlling plantar fasciitis, especially calf mobility. Massage, foam rolling and stretching are all strategies employed to help maintain calf length which can reduce pain, manage the injury and prevent its recurrence in the future.
3. Strength.
At the end of the day, the stronger your calves and feet are, and therefore your tendons and plantar fascia are, the more load they can tolerate and the less chance of them being overloaded. Strength is key in treating plantar fascia, however loading needs to be appropriate for the individual. Strengthening exercises shouldn’t cause pain, or overload the plantar fascia more than it already is. They should replicate and prepare the feet and calves for the type of activity the individual needs to get back to, and be maintained at a certain level to prevent overload occuring again in the future.

How to avoid it
Injuries like this can be challenging to avoid, especially if the triggering factor is something out of your control such as hormones fluctuations, rapid gain in weight similar to what happens in pregnancy, or an unaccounted increase in daily loads. But recognising the warning signs and addressing them immediately, sets you up better for a successful recovery.









